As we see the medical and acute care sector moving toward health and wellness, there’s a sort of equal and opposite reaction moving from the other end of the continuum of health/care: that is, wellness and fitness companies blurring into health care.
Let’s start with the news about CrossFit and 23andMe, then synthesize some key market forces that will help us anticipate more ecosystem change for 2022 and beyond.
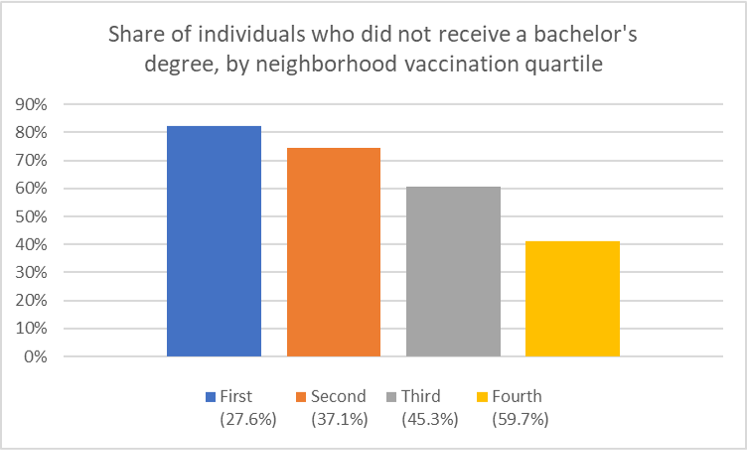
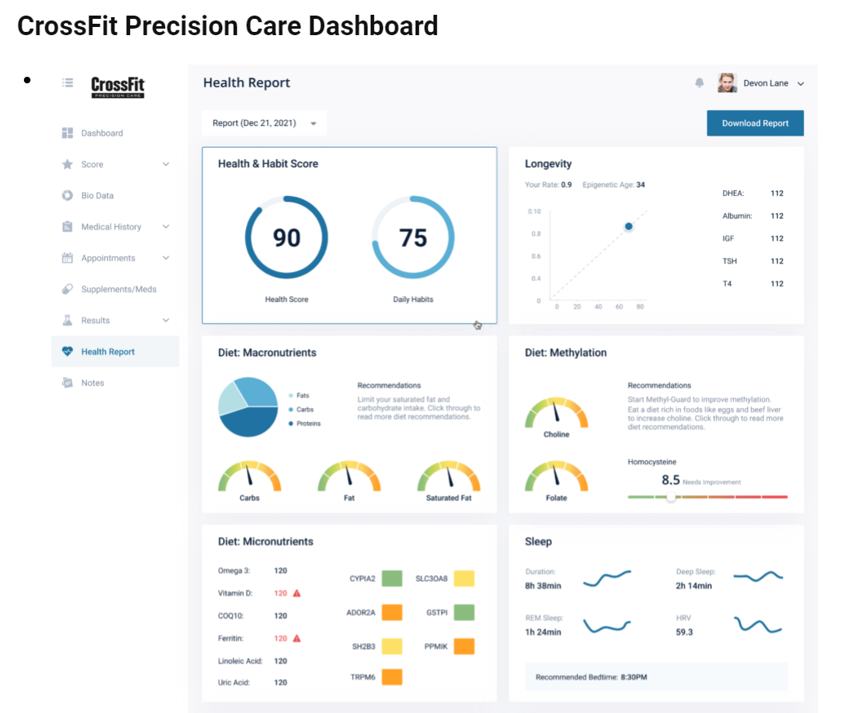
 CrossFit announced the company’s launch of CrossFit Precision Care, described as primary care that provides personalized, data-driven services for “lifelong health,” according to the press release for the program.
CrossFit announced the company’s launch of CrossFit Precision Care, described as primary care that provides personalized, data-driven services for “lifelong health,” according to the press release for the program.
The service is based on four components:
- Genomic testing to identify a consumer’s genetic advantages, disadvantages and predispositions
- Blood testing to assess cardiovascular risks, hormone status, lipids, minerals, thyroid function, and other factors that shape health and performance
- Longevity analysis to estimate a person’s biologic age (using a DNA methylation test kit, adding in the genomic and blood tests), and
- Lifestyle review which formulates eating plans, exercises, family and social life, sleep, hobbies, recreation, and personal goals.
The program was developed by Dr. Julie Foucher and fellow CrossFit-trained physicians collaborating with Wild Health, which has developed what it calls a “platform for personalized medicine” with which the CrossFit Precision Care looks to be linked. Wild Health calls its Clarity algorithm “the world’s first true precision medicine algorithm” applying machine learning to DNA analysis, biometrics, microbiome studies, and phenotype data.
Dr. Foucher, a family medicine physicians, is a former CrossFit Games athlete.
 Speaking of genomic testing….how does 23andMe fit into the health-to-healthcare scenario? The company acquired Lemonaid Health this week, bringing together the consumer-facing genomics company with a prescription drug distribution channel for the purpose of channeling personalized medicine to consumers. This combination is meant to deliver, in the words of 23andme, “individualized primary care that empowers consumers to live healthier lives.”
Speaking of genomic testing….how does 23andMe fit into the health-to-healthcare scenario? The company acquired Lemonaid Health this week, bringing together the consumer-facing genomics company with a prescription drug distribution channel for the purpose of channeling personalized medicine to consumers. This combination is meant to deliver, in the words of 23andme, “individualized primary care that empowers consumers to live healthier lives.”
Lemonaid Health has married prescription drug deliver with telemedicine, one of the group of companies akin to Ro, Hims & Hers, and Nurx, among others.
Anne Wojcicki, the CEO and Co-Founder of 23andMe, explained that the merging of Lemonaid Health’s telehealth platform, underpinned with its team of medical professionals and pharmacy services, will combine with 23andme’s genetics expertise to bring personalized healthcare, “empowering people to take control of their health.”
Together, these two cases — occurring within days of each other — tell us a lot about how U.S. healthcare is accelerating into peoples’ hands, homes, and hearts. The converging factors are:
- Primary care
- Telehealth
- Retail health
- Genetic testing, and
- Collaboration and combination.
It’s that #1 pillar we’ll focus on in the Hot Points, below.
Health Populi’s Hot Points: We only have to look back a matter of here days to understand how profoundly the new-new primary care acceleration is happening. Just last week, Walgreens Boots Alliance announced a doubling down on primary care, mental health services, and telehealth including a $5 billion further investment in VillageMD (giving the company a larger share of the clinic firm). Per the press release, WBA is “reimagining retail through expanded health and wellness offerings and mass personalization.”
CVS Health, which has been building its own primary care vision for several years through the HealthHub, Aetna, and other investments, has a new vision for “SuperClinics” as coined by Karen Lynch, CEO, in a profile of her in Fortune magazine’s Most Powerful Women of 2021.
And, several other news items further paint the current portrait of primary-care-in-motion…
- One Medical’s acquisition of Iora Health
- The launch of Marley Medical, to fill the gaps in primary care for people managing chronic conditions (important to mention initial investors in the company are “OGs” [as the press release says) including digital health pioneers like Anne Wojcicki, David Van Sickle, Halle Tecco, Thomas Goeta, among others who know how to build sustainable digital health ventures}
- Health plans launching “virtual first” plans, such as Humana working with Doctor on Demand, UnitedHealthcare and Optum, Oscar, and Cigna aligned with MDLive, and
- Teladoc’s expanding its virtual primary care program, Primary360, growing from its core telehealth roots,
among many other primary care-focused ventures leveraging virtual care and collaborations.
 Finally, never under-estimate what Amazon Care and the company’s other health care workflows can/will do in primary care.
Finally, never under-estimate what Amazon Care and the company’s other health care workflows can/will do in primary care.
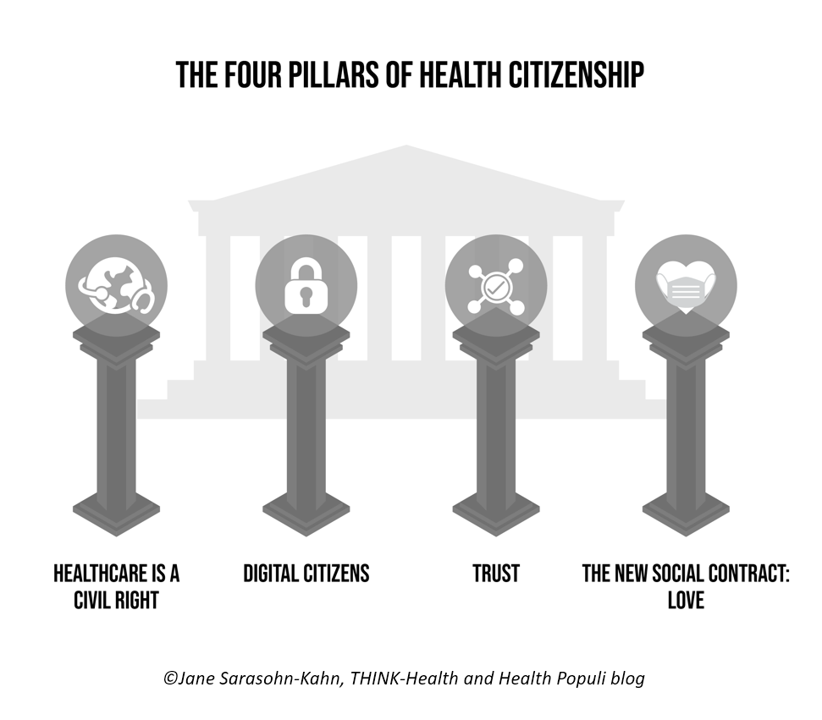
The fact is that nations that invest in resilient, strong primary care backbones ultimately spend less per health citizen than the U.S., with a fragmented on-ramp to primary care for millions of consumers lacking access to upstream, preventive and early-detecting services. This current bullish phrase for new primary care suppliers and business models will add chaos before creation and consolidation where we learn which models work toward the Quintuple Aim.
We will continue to see the mashup and blurring of primary care with personalized medicine, with models built on omnichannel approaches designed for every kind of people if suppliers are design-ful.
The post Why CrossFit and 23andMe Are Moving from Health to Primary Care appeared first on HealthPopuli.com.
Why CrossFit and 23andMe Are Moving from Health to Primary Care posted first on
https://carilloncitydental.blogspot.com

 Speaking of genomic testing….how does 23andMe fit into the health-to-healthcare scenario?
Speaking of genomic testing….how does 23andMe fit into the health-to-healthcare scenario?  Finally, never under-estimate
Finally, never under-estimate