“Yes,” we concurred on our session convened by the American Telemedicine Association (ATA) EDGE session today.
 “We” was a trio including Antoinette Thomas (@NurseTechExec1), Chief Patient Experience Officer with Microsoft, David Ryan (@DavidPRyan), former long-time Global Head of Intel’s Health/Life Science business; and, me.
“We” was a trio including Antoinette Thomas (@NurseTechExec1), Chief Patient Experience Officer with Microsoft, David Ryan (@DavidPRyan), former long-time Global Head of Intel’s Health/Life Science business; and, me.
Antoinette posed three questions for all of us to brainstorm, addressing various aspects of health equity. We covered,
- The theory that telemedicine should increase health equity — where are we and what are the barriers to getting there?
- The role of social determinants of health in creating equitable opportunities for health citizens; and,
- Entering a post-pandemic world, we won’t return to former operational and delivery models. We fast-innovated during the pandemic, so what is possible with what we have learned to avoid further inequities?
In my responses to these questions, I talked about the following, sharing some links with you that underpinned my remarks.
 Understanding the health inequities borne by “telemedicine. As Antoinette posed her question using the noun telemedicine, I parsed the word into its two parts to respond to the question. For “tele,” I noted three aspects of social determinant risk:
Understanding the health inequities borne by “telemedicine. As Antoinette posed her question using the noun telemedicine, I parsed the word into its two parts to respond to the question. For “tele,” I noted three aspects of social determinant risk:
- Connectivity, a person’s lack of access to broadband to the N’th citizen and not just the “last mile”;
- The hardware which provides the on-ramp to a person connecting online, which could be a phone (smart or simple), a tablet, a computer, or a (smart) TV, for example; and,
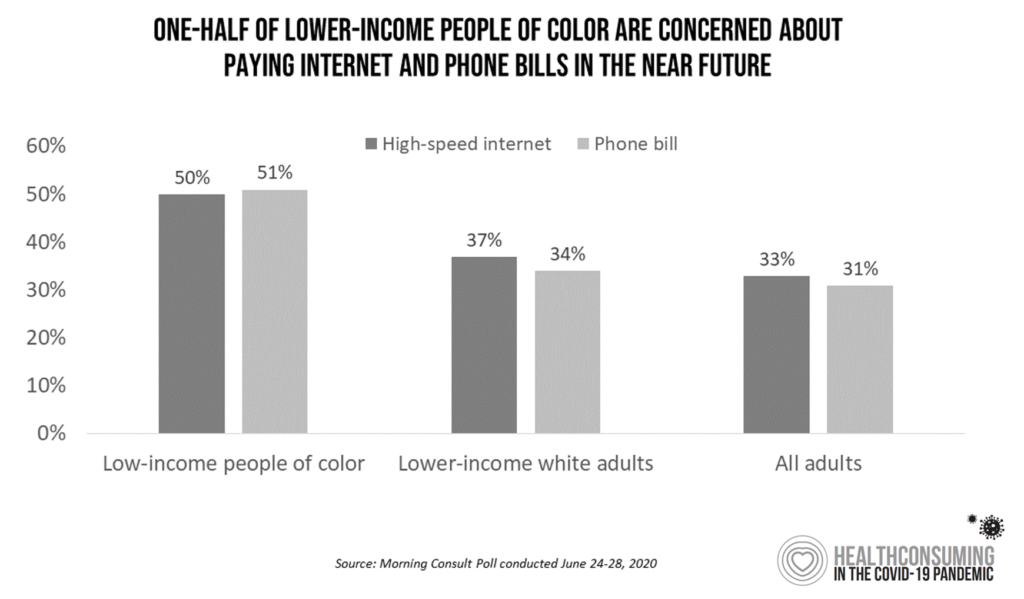
- The data plan that enables a person to make the connection. I noted this Morning Consult survey, data shown here, finding that people of color who were lower-income as of June 2020 had a more difficult time paying for Internet and phone bills than white people with lower incomes.
The second part of the word, “medicine,” has a host of evidence finding health disparities across people of different ethnicities and race, women versus men, and LGBTQ folks. This can be due to historic bias in care and in clinicians’ treatment (which can be conscious or subconscious), how inclusive clinical trial populations have been, or quite in this moment what data are included or excluded from algorithms, along with a host of other issues.
 Social determinants of health: broadband as a “Super Determinant.” With the emergence of the COVID-19 pandemic in the U.S., Americans were mandated to #StayHome, #WorkFromHome, and attend school from home, from elementary through university aged students.
Social determinants of health: broadband as a “Super Determinant.” With the emergence of the COVID-19 pandemic in the U.S., Americans were mandated to #StayHome, #WorkFromHome, and attend school from home, from elementary through university aged students.
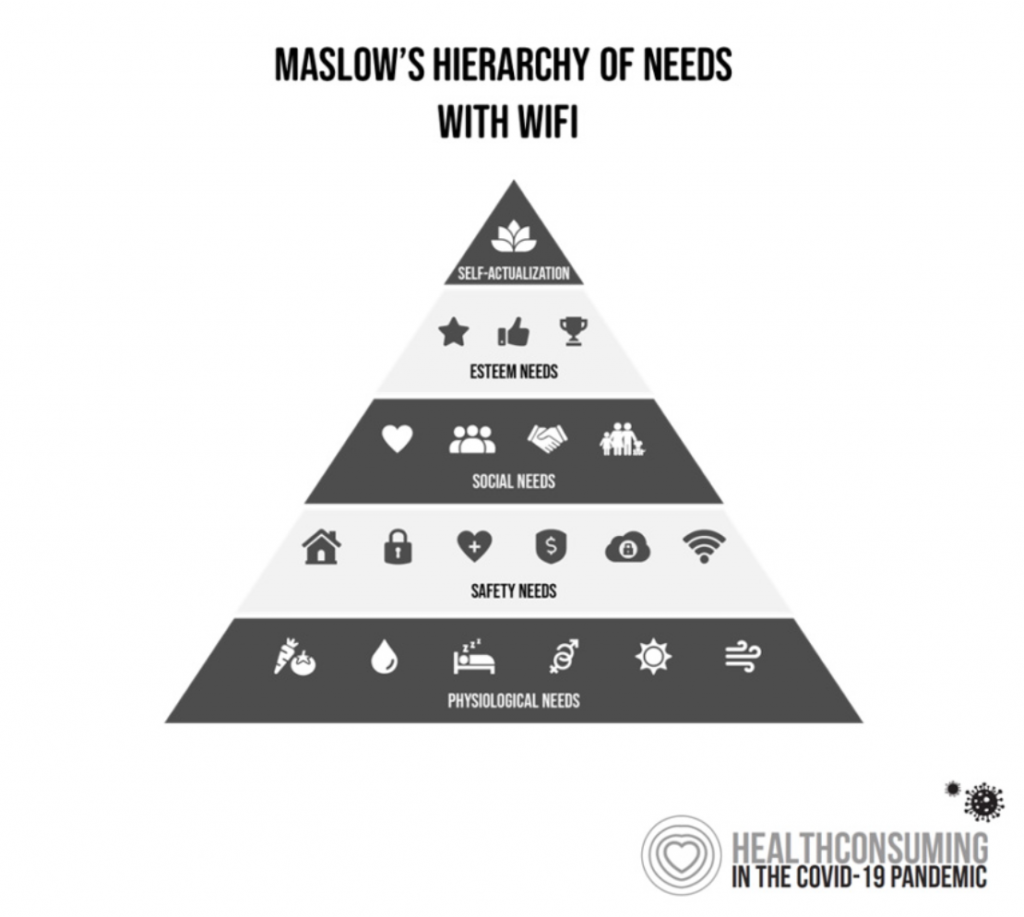
Our personal hierarchies of needs were flattened down to physiological (say, hunting and gathering for food and hygiene supplies) and safety (most importantly, avoiding exposure to the coronavirus).
But connectivity became a Super Determinant of health. I’d called WiFi a social determinant of health in a Huffington Post column I wrote back in 2016, recognizing the emerging virtual health opportunity and potential for furthering the digital divide without bolstering broadband “everywhere.”
The pandemic turbocharged this phenomenon, which was called out by Brittney Crock Bauerly, JD, in a 2018 essay for Network for Public Health Law.
Brittney wrote that, “Lack of broadband access can serve to exacerbate disparities in other social determinants of health, such as by limiting educational and employment opportunities….Job-seekers without broadband at home also face difficulties in looking for work or applying for jobs online….Connectivity also plays an important role in healthcare…Individuals without broadband access may not be able to take advantage of these opportunities for remote care and health promotion.”
 Assuring health equity in a post-pandemic world. As we move to “build health care back better” in the U.S. post-pandemic, we laud the fact that the private sector has been playing a greater role filling in gaps left bare by the public sector in health over the past few years.
Assuring health equity in a post-pandemic world. As we move to “build health care back better” in the U.S. post-pandemic, we laud the fact that the private sector has been playing a greater role filling in gaps left bare by the public sector in health over the past few years.
The retail health landscape, defined broadly, brings services closer to people where they live, work, play, pray, and shop. Retail pharmacy chains and Big Box stores, grocery markets and even convenience stores have been essential touchpoints for peoples’ food, hygiene, and health care supplies from over-the-counter drugs to masks, wearable trackers (sales up in 2020 in part due to the pandemic and greater personal care awareness), and urgent care.
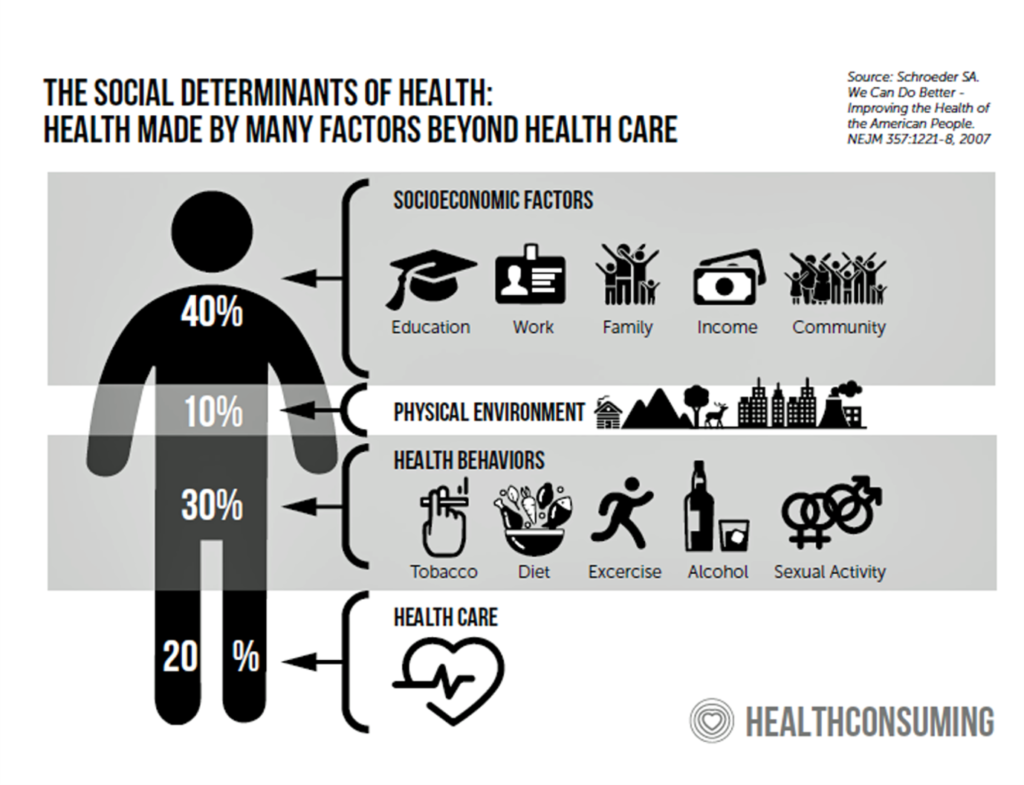
But the private sector cannot craft public policy, which is where a whole-of-government approach is important to address the many social determinants of health at-risk in and beyond the pandemic. Some are shown in this graphic.
We’ve known about the impact and role of SDoH since the age of Hippocrates, and more contemporarily for a couple of decades.
Nothing like a public health crisis to bring new awareness to old knowledge.
 Health Populi’s Hot Points: In Antoinette’s “speed round” concluding our panel, I finished on a philosophical-combined-with-public-policy note. I referred the attendees to an essay penned by Dr. Donald Berwick in a June 2020 JAMA titled, The Moral Determinants of Health.
Health Populi’s Hot Points: In Antoinette’s “speed round” concluding our panel, I finished on a philosophical-combined-with-public-policy note. I referred the attendees to an essay penned by Dr. Donald Berwick in a June 2020 JAMA titled, The Moral Determinants of Health.
In this viewpoint, Dr. Berwick considered the first few months into the COVID-19 pandemic, recognizing the disparities in health outcomes for different people living in America. He referred to the research of Sir Michael Marmot in the UK on social determinants, who segmented these in terms of conditions of birth and early childhood, education, work, the social circumstances of elders, community resilience indicators (like transportation, housing, security), and “fairness.”
However we define them, these factors impact health much more than medical interventions applied downstream.
 “How do humans invest in their own vitality and longevity?” Berwick asks. The answers seems illogical in wealthy countries, he notes, as most dollars in the U.S. go to the “expensive repair shops” — that is inpatient hospital care and emergency services.
“How do humans invest in their own vitality and longevity?” Berwick asks. The answers seems illogical in wealthy countries, he notes, as most dollars in the U.S. go to the “expensive repair shops” — that is inpatient hospital care and emergency services.
At the same time, much smaller spend goes to prevent damage — such as homelessness, hunger, and mental illness.
Dr. Berwick explains the concept of moral law, begging the question: what is health care’s “lane?”
“Healers are called to heal,” he concludes his essay. “Improving the social determinants of health will be brought at last to a boil only by the heat of the moral determinants of health.”
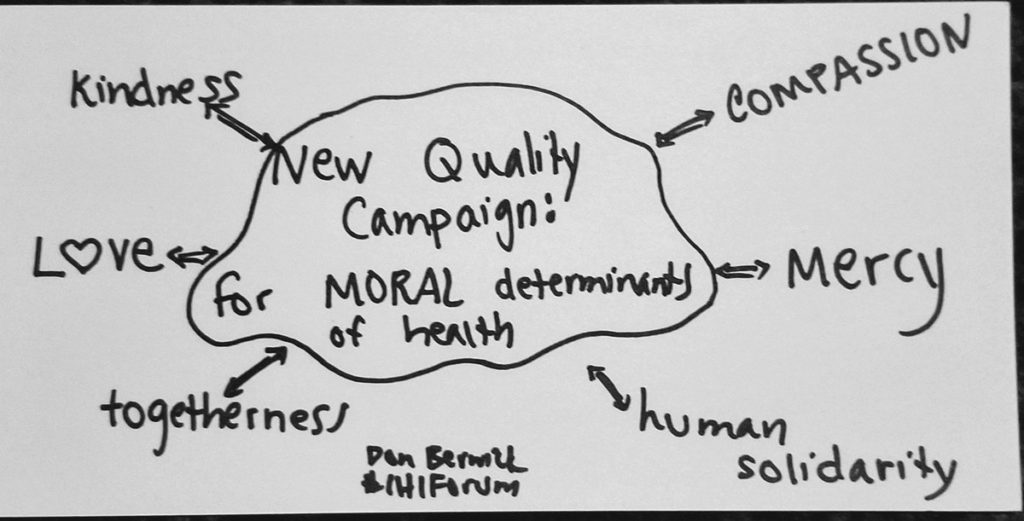
Here is a graphic snapped from a Don Berwick #IHIForum discussing the moral determinants of health. This was drawn in the context of developing a new quality health care campaign baking in the moral determinants of health.
What would such a strategy address? Human solidarity, togetherness, kindness, compassion, mercy, and….love, part of a new social contract for health.
Thanks to my collaborators, Antoinette and Dave, demonstrating all these traits in our ATA session.
Special thanks to the ATA, CEO Ann Mond Johnson and Dr. Joseph Kvedar, ATA President, for inviting us to cover this important topic at this pivotal time for U.S. health care and the nation’s health citizens.
The post Can Telemedicine Increase Health Equity? A Conversation with Antoinette Thomas, Dave Ryan, and Me with the ATA appeared first on HealthPopuli.com.
Can Telemedicine Increase Health Equity? A Conversation with Antoinette Thomas, Dave Ryan, and Me with the ATA posted first on https://carilloncitydental.blogspot.com
No comments:
Post a Comment