 Over the next 20 years, health care spending in the U.S. will migrate toward well-being and the early detection of disease, away from the funding of America’s sick-care system, according to Breaking the cost curve, a forecast of U.S. health economics in the year 2040 from Deloitte.
Over the next 20 years, health care spending in the U.S. will migrate toward well-being and the early detection of disease, away from the funding of America’s sick-care system, according to Breaking the cost curve, a forecast of U.S. health economics in the year 2040 from Deloitte.
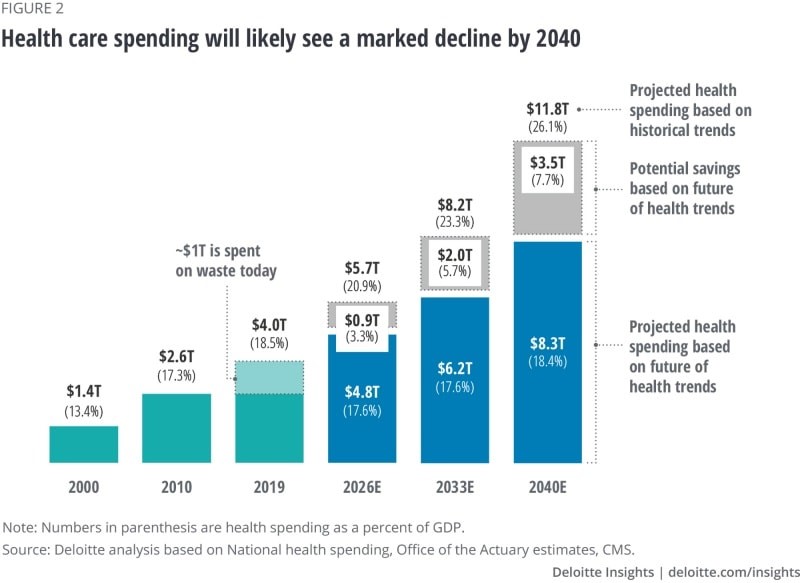
Current spending on health care in America is roughly $4 trillion (with a “t”) dollars, approaching 20% of the nation’s economy.
By 2040, spending is projected to be $8.3 trillion based on future health trends — not historic workflows and delivery mechanisms which would consume an additional $3.5 trillion — close to what we are spending today.
Interestingly that $8.3 trillion spend represents about the same proportion of today’s health care spending, roughly $1 in $5 of national spending.
Deloitte’s analysis is something of a contrarian view given the never-ending upward cost-curve that has been stubborn to bend for decades.
The COVID-19 pandemic has, in fact, had a positive impact on spending per se given the volume-based nature of U.S. health care and that volumes turned downward in 2020.
 But letting a virulent public health crisis manage the downturn in American health spending is hardly an optimal hands-on, strategic approach to improving a nation’s health system, let alone a vision to drive health equity, quality improvement and sustainability for patients and care providers.
But letting a virulent public health crisis manage the downturn in American health spending is hardly an optimal hands-on, strategic approach to improving a nation’s health system, let alone a vision to drive health equity, quality improvement and sustainability for patients and care providers.
Deloitte’s actuaries actually developed this analysis using data from before the coronavirus pandemic.
The top-line is that technology innovations, early disease detection and prevention, and consumer health engagement will together control costs and pivot the sick-care system to one focused on well-being.
Deloitte points to three “future realities” in their modeling:
- A $3.5 trillion “well-being dividend,” those cost-savings generated by the shift toward prevention and early disease detection and the adoption of (appropriate, cost-effective) technologies
- Shifting spending toward well-being and social determinants of health earlier in health citizens’ life cycles
- A new health economy bringing about the “end of the general hospital as we know it,” a dramatic change in health care financing in the U.S., and a slowing of mass/general pharma manufacturing.
The second chart shows six developments that drive the future state of health care and spending in the U.S., including data sharing enabling better care coordination; interoperability resulting in price transparency and smarter spending on what works; equitable access shifting care to lower-cost, accessible settings away from capital-intensive inpatient care; empowered well-being, putting work-flows into patient-consumer-citizen hands as people “take ownership of health;” behavior change which is driven by behavioral economics; and, scientific breakthroughs focused on health-economic outcomes research and personalization.
 Health Populi’s Hot Points: Deloitte is expecting “seismic shifts” over the next twenty years as the U.S. health economy moves from sick care to a system focused on well-being.
Health Populi’s Hot Points: Deloitte is expecting “seismic shifts” over the next twenty years as the U.S. health economy moves from sick care to a system focused on well-being.
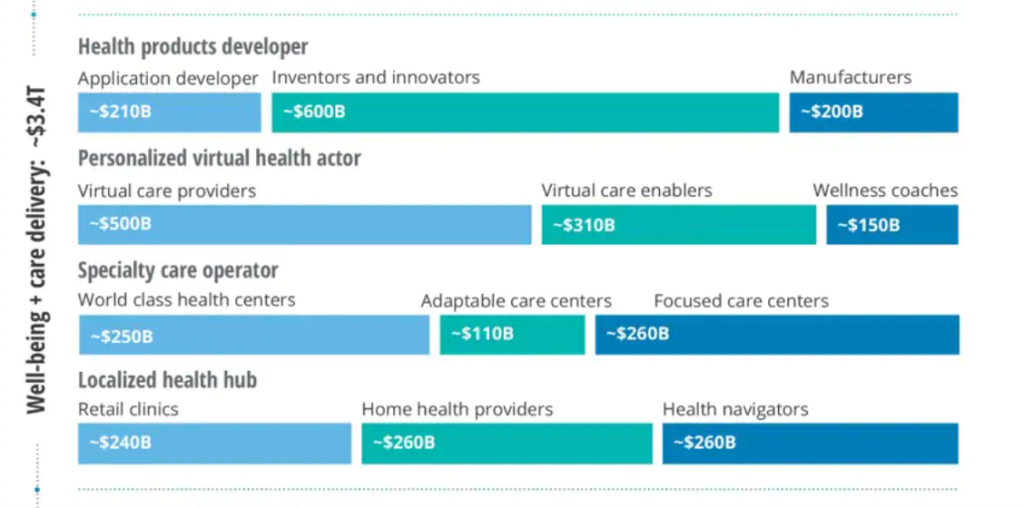
The biggest shift in this scenario is that $4 in $10 would be allocated to well-being and care delivery, and $3 in $10 for data + platform that informs cost-effective care.
This last chart comes out of Deloitte’s projections for three key components in the U.S. health care system for 2040, focusing on just the well-being + care delivery segment (the other two are the data + platforms, and care enablement segments).
This component breaks down into four categories of work flows and spending by persona or “new business archetype”/actor:
- Health products developers, with most spending going to inventors and innovators followed by application developers and manufacturers
- Personalized virtual health actors including virtual care providers, enablers, and wellness coaches
- Specialty care operators, featuring focused care centers, world class health centers, and adaptable care centers, and
- Localized health hubs such as retail clinics, home health providers, and health navigators.
There’s nary a “hospital” to see in this scenario. There are those care centers which are specialized, and local health hubs.
The COVID-19 pandemic revealed many weaknesses in U.S. health care as it is currently organized, financed, and delivered. Health inequities and disparities, volume-based payment, and inaccessible, unhygienic physical plants were some of the areas the public health crisis highlighted for us to learn and grow from in re-imagining and re-building a more equitable, cost-effective, and safer health care system in America.
 The value of care delivered at home and closer-to-home is part of this awareness, which is represented by the re-envisioned care delivery modes in Deloitte’s vision here. Deloitte provides a provocative argument for how to bend America’s unsustainable health care cost curve while enabling patients – morphing from consumers to health citizens “owning their care and health,” in Deloitte’s words.
The value of care delivered at home and closer-to-home is part of this awareness, which is represented by the re-envisioned care delivery modes in Deloitte’s vision here. Deloitte provides a provocative argument for how to bend America’s unsustainable health care cost curve while enabling patients – morphing from consumers to health citizens “owning their care and health,” in Deloitte’s words.
I share that vision with Deloitte, explained in my book, Health Citizenship — where we envision people “owning and not renting” their health and health care.
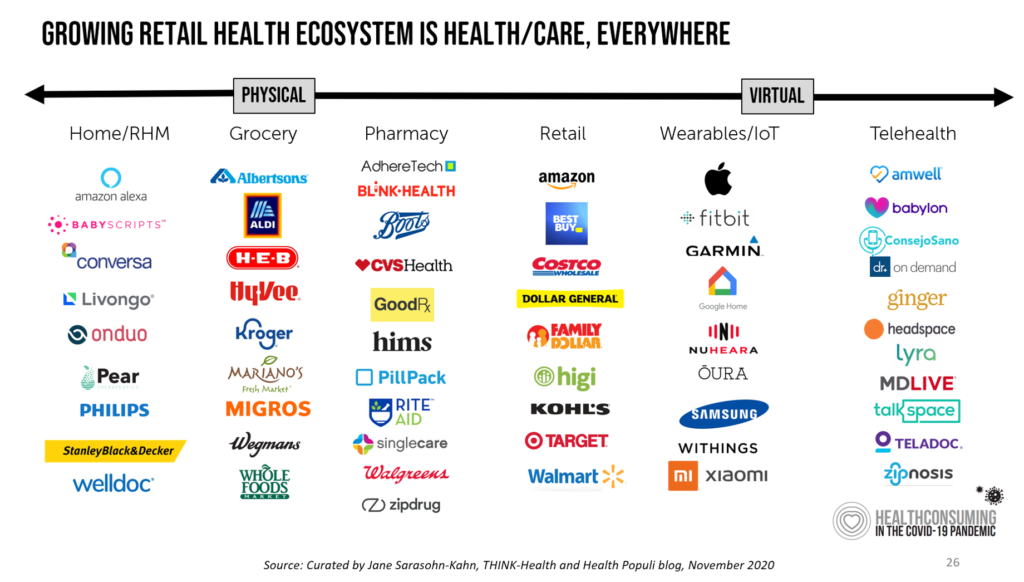
The past few years have birthed a growing roster of organizations serving up new models for primary care: the list includes CVS/health, Walgreens coupled with VillageMD, Walmart and its evolving approach to community-based primary care, and many new models for primary care targeting specific populations (from working age employed people to older folks in Medicare Advantage plans providing food and social determinants-focused services), among others.
U.S. hospitals have taken a huge hit — financial and in terms of human capital front-line clinicians — in the COVID-19 pandemic. Their ability to recover in 2021 and 2022 as the national economy heals and again grows will be a crucial time period to strategic plan and executive for a future that is not defined by a traditional inpatient bed.
The post The Health Care Cost Curve is Bending Down – A New View from Deloitte appeared first on HealthPopuli.com.
The Health Care Cost Curve is Bending Down – A New View from Deloitte posted first on https://carilloncitydental.blogspot.com
No comments:
Post a Comment