The COVID-19 pandemic forced consumers to define what were basic or essential needs to them; for most people, those items have been hygiene products, food, and connectivity to the Internet.
 There’s another good that’s essential to people who are patients: prescription drugs. A new report from CoverMyMeds details the current state of medication access weaving together key health care industry and consumer data.
There’s another good that’s essential to people who are patients: prescription drugs. A new report from CoverMyMeds details the current state of medication access weaving together key health care industry and consumer data.
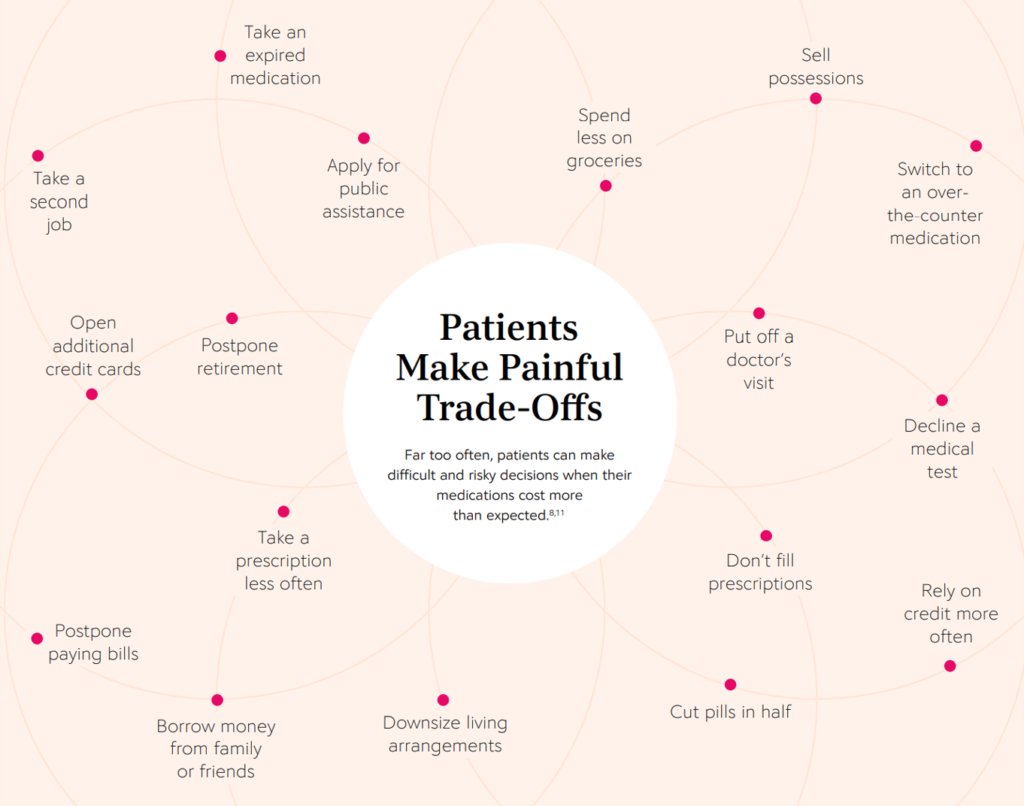
The reality even before the coronavirus crisis emerged in early 2020 was that U.S. patients were already making painful trade-offs, some of which are illustrated in the first chart from the report. These include self-rationing prescription drug fills or refills due to cost, putting off a doctor’s visit, relying more on credit cards than cash, and postponing paying bills, among many other choices between paying for meds or daily living expenses.
One in three patients went without treatment or medications to pay for bills and basic needs, the research found. Those patients trying to stay medication-adherent tried various strategies such as stretching out their prescriptions, skipping doses, or reducing those doses — not sticking to the prescribed regimen, which can result in an adverse event or compromise the intended health outcome.
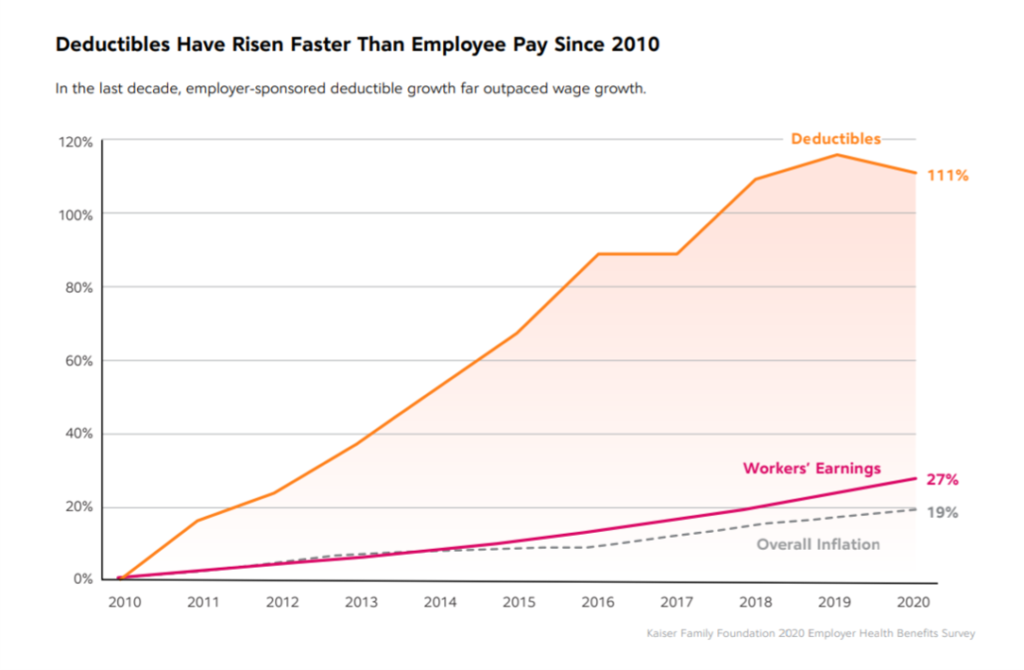 One basic pillar of prescription drug access is health care insurance; CoverMyMeds points out that unemployment claims hit record (high) levels in 2020, with millions having lost health coverage. For those with health benefits, the report points to this powerful Kaiser Family Foundation chart that illustrates the huge gap between the rise of the cost of high-deductibles compared with the fairly flat picture on worker earnings growth.
One basic pillar of prescription drug access is health care insurance; CoverMyMeds points out that unemployment claims hit record (high) levels in 2020, with millions having lost health coverage. For those with health benefits, the report points to this powerful Kaiser Family Foundation chart that illustrates the huge gap between the rise of the cost of high-deductibles compared with the fairly flat picture on worker earnings growth.
This is the concept that, for some patients with health insurance, they feel “under-insured” in that they cannot afford to pay to meet their insurance deductible, thereby forgoing health care (including filling prescription drugs).
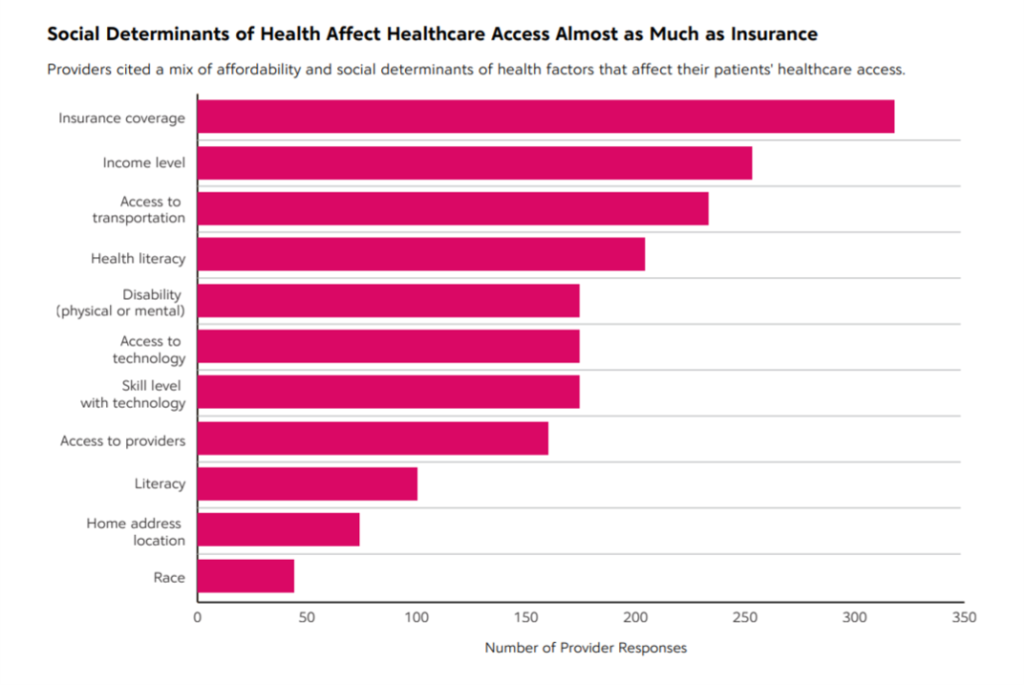 In addition to affordability and insurance coverage, CoverMyMeds also points to various social determinants of health that can impact a person’s access to health care/medicines, shown in this chart from their research. One’s income level, access to transportation, health literacy, disability, access to technology as well as efficacy in using that technology, and access to providers were top social determinant risks cited by providers in this study.
In addition to affordability and insurance coverage, CoverMyMeds also points to various social determinants of health that can impact a person’s access to health care/medicines, shown in this chart from their research. One’s income level, access to transportation, health literacy, disability, access to technology as well as efficacy in using that technology, and access to providers were top social determinant risks cited by providers in this study.
CoverMyMeds then details social inequities that were clearly uncovered during the COVID-19 pandemic, though persistent over decades in the U.S.
Racial minorities were more adversely financially impacted by COVID-19, the survey learned:
- 78% of people who were racial minorities were financially impacted by COVID-19 compared with 54% of White people
- 45% of people in racial minorities had to forgo treatments or medications to pay for other essential items versus 21% of Whites
- 56% of racial minorities had to forgo paying for essential items to afford treatments or medications
- 53% of racial minorities had to modify treatment to stretch out prescriptions, such as take a lower dose or skip one.
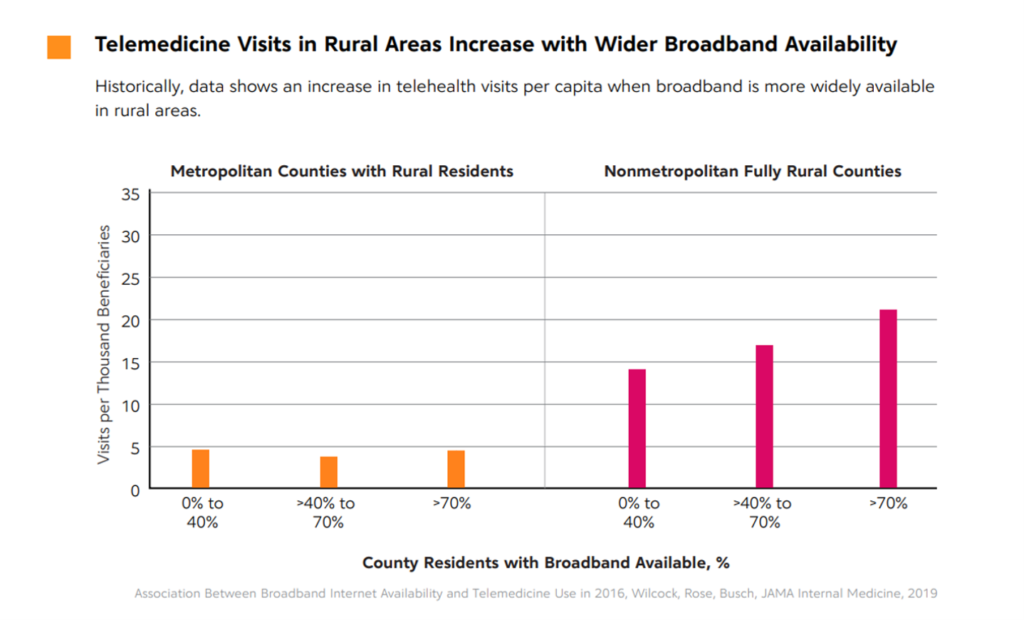 Another social determinant not typically on the list of such risks is connectivity and access to broadband. As the COVID-19 crisis led to large parts of the U.S. economy shutting down in the first and second quarters of 2020, health care providers pivoted to telehealth and virtual care platforms. At the same time, patients were keen to risk-manage their exposure to the virus, so wanted to stay home and not visit providers’ offices if they were open to appointments.
Another social determinant not typically on the list of such risks is connectivity and access to broadband. As the COVID-19 crisis led to large parts of the U.S. economy shutting down in the first and second quarters of 2020, health care providers pivoted to telehealth and virtual care platforms. At the same time, patients were keen to risk-manage their exposure to the virus, so wanted to stay home and not visit providers’ offices if they were open to appointments.
Those patients who did not have access to broadband were out-of-luck in seeing clinicians at-a-distance and receiving necessary care that was available to other health consumers who could go online.
This further exacerbated the un-connected patients’ ability to work-from-home if that was an option for them, or attend school at home which millions of students from elementary through college age were forced to do.
Note that 80% of providers said that even when patients had access to digital technology as an on-ramp to telehealth visits, consumers’ lack of skills using the technology was a barrier to convening with patients online.
For this research, CoverMyMeds surveyed 1,000 patients, 400 providers, and 328 pharmacists in September and October 2020.
 Health Populi’s Hot Points: The shift to telehealth will persist post-pandemic, into 2022, the extent of which will depend on two key uncertainties in this moment:
Health Populi’s Hot Points: The shift to telehealth will persist post-pandemic, into 2022, the extent of which will depend on two key uncertainties in this moment:
- How payors will set reimbursement/payment levels for virtual care, both public sector (Medicare, Medicaid, VA) and commercial health plans; and,
- The pace of the rate of update by providers taking on value-based payment in their organizations.
As providers accept value-based payment, they have an incentive to adopt digital health tools that empower patients to align with them, virtually and economically. Telehealth, remote health monitoring to the home, and patients’ use of wearable tech and consumer-facing health devices can shift more care to the home and into patients’ hands, lowering the cost of care to the provider paid on value and at the same time, ensuring that patients receive necessary care underpinned by patient-centered design that takes into account their personal circumstances including risks due to social determinants of health — including broadband connectivity.
The last charge shows that one-half of providers grew telehealth appointments and decreased face-to-face appointments. At the same time, some providers saw a decrease in compliance to therapy, which must be bolstered through more effective patient engagement programs, health literacy education, and potentially the use of digital tools to remind and “nudge” people to take their meds. At the same time, if on the patient-consumer side, medication costs are a barrier to adherence, then the provider should partner with pharma companies to link patients to access programs that can benefit those people for whom the cost of meds is a bridge too far (and expensive) to cross.
The CoverMyMeds report is a wide-ranging work covering other important issues than I’ve captured in this post, focusing on patient access to medicines as a social determinant. This is highly-recommended reading to help us put medications and drug economics in the context of COVID-19 and beyond the pandemic.
The post The Social Determinants of Prescription Drugs – A View From CoverMyMeds appeared first on HealthPopuli.com.
The Social Determinants of Prescription Drugs – A View From CoverMyMeds posted first on https://carilloncitydental.blogspot.com
No comments:
Post a Comment