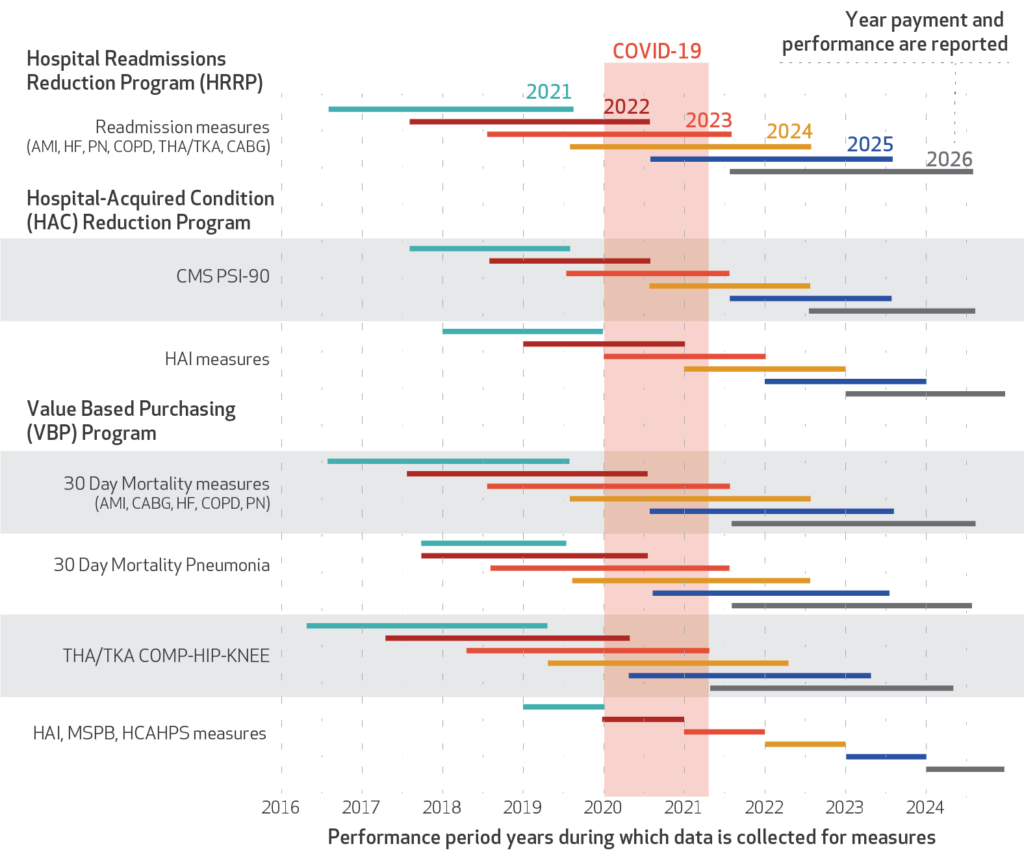
Many Medicare payment initiatives aim to link reimbursement to value. Value includes both cost and quality of care. However, measuring quality of care during a pandemic is problematic. Further, most of CMS’ value-based purchasing programs–such as Hospital Value-Based Purchasing (VBP) Program, the Hospital Readmissions Reduction Program (HRRP) and the Hospital-Acquired Condition (HAC) Reduction Program all look at retrospective data to evaluate quality. From the chart below (courtesy of the Salzberg and Khan piece in the Health Affairs blog) one can see that quality impacts during COVID-19 will affect Medicare reimbursement to providers through 2024 for most programs and in some cases through 2025.
https://ift.tt/3oQJNOB
There are a number of issues with the data during COVID-19.
- Data reporting quality. CMS granted reprieves and attempted to mitigate quality measure reporting burden for many health care providers. While this is a wise an sensible approach in the midst of a pandemic, it also means that data quality may be worse than in other years. For instance, one could observe a drop in quality during COVID-19 years, not due to worse quality, but rather simply due to quality reporting.
- Dealing with COVID-19. Clearly, prior to 2020 there were no quality measures related to quality of COVID care. Thus, even if a hospital provided great COVID-19 care, they would not get credit for that under existing value-based purchasing systems as there were not measures to quantify this dimension of quality. Further, there were new challenges hospitals and other providers had to deal with including additional cost for personal protective equipment (PPE) and infection control protocols.
- Capacity constraints. With so much effort used to deal with COVID-19, there was less be space and staff available for treating other patients with other diseases.
- Case mix during COVID-19. During the peaks of the pandemic, many individuals did their upmost to avoid going to the hospital. Thus, most people who went to the hospital during COVID-19 were those who had no other choice. Thus, one would expect the acuity of non-COVID patients admitted to hospitals during the pandemic to be more severe than normal.
- Case mix after COVID-19. The case mix of patients after COVID-19 may also be more severe. Some individuals may have put off getting preventive or maintenance care during the pandemic; others may have put off needed surgeries. Thus, patients after the pandemic may also present with more acuity due to decisions to put off needed care.
In short, the data on quality of care during the pandemic is unlikely to be comparable to previous or subsequent years. These issues pose a challenge to payers to make reimbursement fair, while continue to rewarding high-value care. Salzberg and Khan conclude by saying:
While the full impact of COVID-19 on hospitals and health systems is yet to be understood, understanding the specific impact and predicting effects on data can help direct analyses, ensure we do not mislead patients with invalid data, nor incorrectly penalize hospitals for delivering care during a period of duress for which we cannot know the extent of the impact.
Impact of COVID-19 on CMS’ value-based programs posted first on https://carilloncitydental.blogspot.com
No comments:
Post a Comment