This is the question posed by a recent article by Lopata et al. (2021). The authors surveyed 26 payers (e.g., leaders of national, regional, local, Medicaid, and Medicare plans; payer components of integrated delivery systems; and pharmacy benefit managers (PBMs) and 11 employers (e.g., large employers, employee benefit consultants, employer coalitions). Respondents were informed that orphan disease was defined as “a condition that affects fewer than 200,000 people in the United States.”
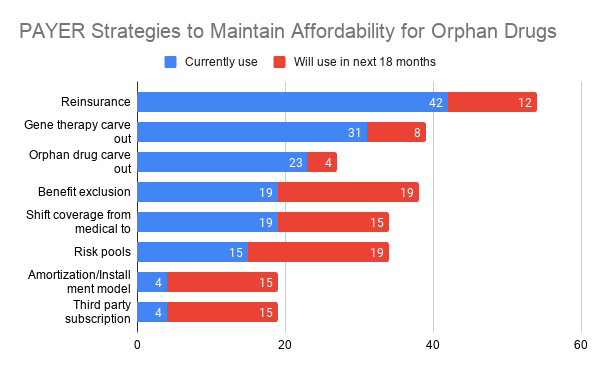
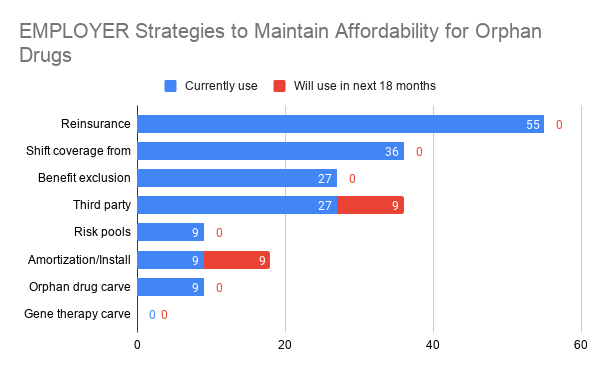
Most payers used resinurance (42%), a gene therapy carve-out (31%) or orphan drug carve-outs (23%). While employers also favored the use of reinsurance (55%), use of carve outs was rare and shifting benefits from medical to pharmacy coverage (36%) or benefit exclusions (27%) or third party subscription models (27%) were more common.
Are limited distribution networks the answer? Payers didn’t think so.
More than three fourths (76%) of respondents indicated that limited distribution networks impede management, with only 4% indicating that they improve management.
Another key question is whether to cover health care provider (HCP)-administered orphan drugs under a medical or a pharmacy benefit. There are reasons that justify both options.
The top factors that drove payer coverage of HCP-administered orphan drugs to the medical benefit were site-of-care policies (55%), lower-drug cost through average sales price (ASP) pricing (50%), preference of network providers (35%), and patient afford-ability (20%). The top factors that drove payer coverage of HCP-administered products to the pharmacy benefit were improved ability to manage product (71%), rebates (62%), ability to leverage resources from specialty pharmacy pro-viders (SPP; 57%), site-of-care policies (52%), improved data granularity (38%), preference of network providers (38%), and patient affordability (24%)…
The development of new treatments for rare diseases is one we should welcome, as these patients need treatment. At the same time, payers and employers are likely to continue exploring creative strategies for making coverage of these treatments affordable.
- Lopata E, Terrone C, Gopalan A, Ladikos N, Richardson T. Meeting the affordability challenges posed by orphan drugs: a survey of payers, providers, and employers. Journal of Managed Care & Specialty Pharmacy. 2021 Feb 15:1-8.
Which strategies are payers and employers using to cover orphan drugs? posted first on https://carilloncitydental.blogspot.com
No comments:
Post a Comment