Many of us who are patients have the unpleasant experience of navigating the complex world of drug utilization management. This includes determining what formulary tier a drug will be on, if there are any prior authorization requirements and what our copay will be. The burden also falls on physicians in that they need to justify why specific drugs are needed for a given patient to secure coverage. Drug companies also have costs for programs to help patients and physicians navigate the utilization management programs, rebates, free samples, and co-payment assistance. Payers also have the additional cost of administering these utilization management programs. The fact that utilization management imposes costs on a variety of stakeholders is not surprising. In fact, the goal is to impose costs on different stakeholders to incentivize the use of lower cost medications. One unanswered question, however, is how large these costs actually are.
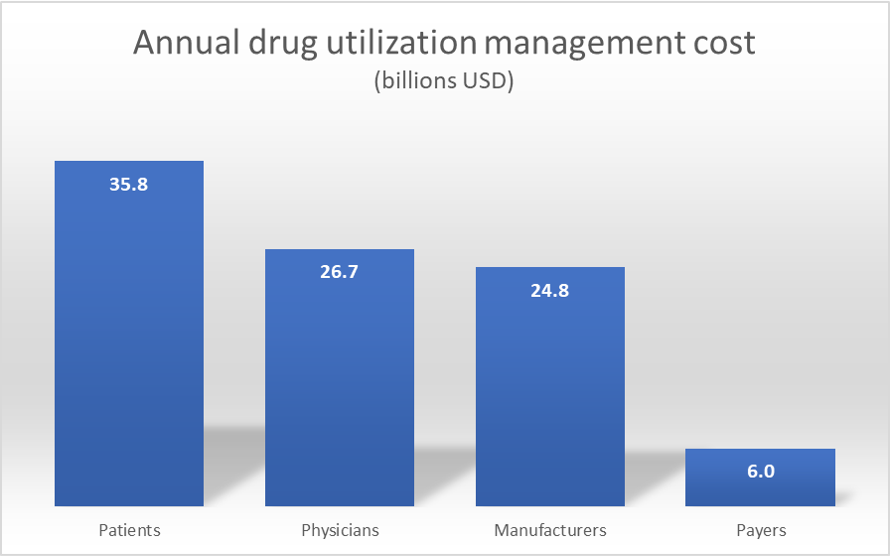
A recent paper in Health Affairs by Howell, Yin and Robinson, find that the annual cost in the US is $93.3 billion. Patients bear the largest burden at $35.8 billion with physicians ($26.7 billion) and manufacturers ($24.8 billion) coming in at second and third place. Payers cost is much smaller but not trivial at $6.0 billion.
The authors reach these conclusion by conducting a literature review of peer-reviewed studies published between 2009 and 2020 supplemented by other news articles.
The authors argue one solution to the utilization management arms race, would be for manufacturers to price drugs based on treatment value in exchange for PBMs/payers to allow “value-based access” with minimal utilization management restrictions. While sensible, identifying an appropriate notion of “value” is often challenging. However, removing barriers to patient access is a laudable goal.
Cost of drug utilization management is over $90 billion per year posted first on https://carilloncitydental.blogspot.com
No comments:
Post a Comment